Colon cancer is the third most common cancer, behind prostate cancer in men and breast cancer in women, according to Dr. Anoop K. Shah, director of the gastroenterology department at St. Mary Medical Center – Dignity Health. In February 2000, President Clinton dedicated March as National Colon Cancer Awareness Month.
According to cancer.org, more than 130,000 new cases of colorectal (colon and rectal) cancer and 50,000 deaths are expected in the United States alone in 2017. However, if screened for properly, colon cancer is preventable and treatable.

Dr. Anoop K. Shah, director of the gastroenterology department at St. Mary Medical Center – Dignity Health in Downtown Long Beach, said colon cancer is the third most common cancer but that it is preventable if patients follow recommended screening practices, which include receiving regular colonoscopies beginning at age 50. (Photograph by the Business Journal’s Larry Duncan)
“Probably close to 50% of people are not getting the screening they need,” Shah said. “Three to five years ago, if I gave a lecture it would be up to 60% of people are not getting the screening they need. We’re seeing in the last few years a tremendous drop in colon cancer diagnosis.”
While Shah said the increase in awareness is a good sign, there is still a lot of work to be done to reach more patients and lessen the number of colon cancer diagnoses. According to Shah, the leading factor for the increase in screenings is that under the Affordable Care Act (ACA), colonoscopies – the most tried and true screening procedure for colon cancer – is 100% free through all insurance companies.
According to Shah, the ACA includes a mandate that requires all insurance companies to cover certain procedures free of charge regardless of the health care plan deductible. The procedures covered are all preventative, including mammograms, pap smears, physicals and colonoscopies, among a few others.
“The government . . . has really made this easier on the patient,” Shah said. “This is a preventative test that’s accepted in a wide body of literature. And for the longest time, insurances weren’t paying for it or were only partially paying for it, which was counterintuitive to the whole premise of preventative care.”
To ensure customers know these preventive procedures are free, Shah said the government randomly audits health care providers to ensure at least 60% of eligible patients were offered them. Shah said his waiting room is often filled with patients holding reminder letters from insurance companies to schedule a colonoscopy.
Around 95% of colon cancer begins as small polyps in the colon that can be easily detected during a colonoscopy, according to Dr. Conrad A. Cox, a gastroenterologist affiliated with Lakewood Regional Medical Center. Patients are sedated for the procedure, which only lasts between 15 and 20 minutes. A flexible fiber-optic instrument called a colonoscope is fitted with a light and camera and is inserted into the colon to allow doctors to detect polyps that may have formed.
The day before the procedure, patients are put on a special liquid diet to cleanse the colon. Cox said many people find the procedure preparations more difficult and uncomfortable than the actual procedure itself, considering the sedation.
“Polyps are a precursor to cancer, and we find these polyps in about one-quarter of patients,” Cox said. “If we find one or two small polyps, then the recommendation is the next [screening] would be in five to 10 years. If we find three polyps, then we’re thinking the potential for that particular colon to develop these polyps becomes greater, so we increase the intervals.”
If more than four or five polyps are found during a screening, Cox said it might be recommended that the next screening be done the following year. When it comes to screenings, Cox admitted that while the colonoscopy is the most effective, it is invasive and can be inconvenient. So some patients may not want or cannot have the procedure. However, there are several other options for patients.
Kaiser Permanente offers two other screening procedures that are less invasive than the standard colonoscopy, according to Kaiser gastroenterologist Dr. Kapil R. Mehta. However, he said that each test must be conducted more often, and if there is a positive result, the patient will have to undergo a colonoscopy anyway.
The least invasive alternative is testing for blood in a stool sample. Mehta said the sample could be small and even taken off tissue paper after wiping. It is recommended the test be conducted every year.
Mehta said Kaiser also offers a sigmoidoscopy, which is a less invasive version of a full colonoscopy, where the scope is inserted into the rectum and examines the left portion of the colon. The idea is that if the left portion is clear of polyps, it is very likely the rest is clear also.
Regardless of the type of screening, if multiple small polyps are discovered in the colon, they can be removed easily during a colonoscopy without surgery. If the lesions are larger, doctors will often take a biopsy to determine if they are cancerous. Benign lesions would be removed, and the patient would continue screenings at shorter intervals. With cancerous lesions, Mehta said a CAT scan could be used to stage the cancer and check for spreading.
“If there’s no spread, which two out of three times is usually the case, then surgery would be an adequate removal. You’d remove that section of the colon and then reattach,” Mehta said “That retains the integrity of the colon and, at the same time, removes the cancer portion of it.”
If cancer cells have spread to adjacent lymph nodes or anywhere else outside the colon, Mehta said the original tumor would be surgically removed from the colon and chemotherapy would be used to eradicate the remaining cancer cells. However, he pointed out that regular screenings often catch polyps before they become cancerous or shortly after, which greatly reduces the likelihood of spreading and increases the chances of survival.
“The survival rate actually ranges from 90% to 100% if we catch it early enough and it’s removed,” Dr. Bhavesh B. Shah, medical director of interventional gastroenterology at Long Beach Memorial Medical Center, said. “Unfortunately, the numbers are not great if we catch the disease later in the process. Some of the studies show the survival rate drop to between 5% and 10%.”
Bhavesh said the drastic decrease in survival rates is a testament to the importance of screening for colon cancer. He said it is one of only a few diseases that can be prevented if appropriate guidelines are followed, namely getting screened at the recommended ages.
For most people, colon cancer screenings are suggested at age 50 and every 10 years thereafter until age 75, unless an excess of polyps or cancer forms, which would result in more frequent screenings. Several exceptions include those who have a family history of colon cancer, people suffering from obesity and African-Americans, who should begin screenings around age 45, according to Bhavesh.
Several risk factors have been linked to or associated with colon cancer, including obesity, alcohol consumption, tobacco use and high-fat diets. Bhavesh acknowledged that these links are not fully proven or backed by comprehensive studies. However, he pointed out that these habits are known to cause several other ailments, so avoiding them keeps people healthier regardless of the link to colon cancer.
Symptoms of colon cancer that should be recognized between screenings – or even before a person reaches the recommended screening age – include blood in the stool, abdominal pain, unexplained weight loss and a change in bowel movements, including constipation.
“I don’t consider March as the only month that we focus on this,” Mehta said. “In today’s day and age, it just makes no sense that we would see as many colon cancers as we do. I think that raising awareness is a huge thing.”
From The American Cancer Society
The Normal Colon And Rectum
The colon and rectum are parts of the digestive system, which is also called the gastrointestinal (GI) system (see illustration). The colon and rectum make up the large intestine (or large bowel). Most of the large intestine is made up of the colon, a muscular tube about 5 feet long. The colon absorbs water and salt from the remaining food matter after it goes through the small intestine (small bowel).
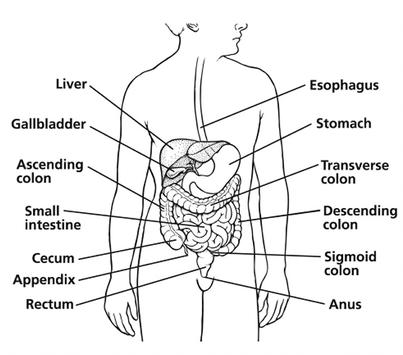
The waste matter that is left after going through the colon goes into the rectum, the final 6 inches of the digestive system, where it is stored until it passes out of the body through the anus.
Types Of Cancer In The Colon And Rectum
Adenocarcinomas make up more than 95% of colorectal cancers. These cancers start in cells that form glands that make mucus to lubricate the inside of the colon and rectum. When doctors talk about colorectal cancer, they are almost always talking about this type.
Other, less common types of tumors can also start in the colon and rectum. These include:
Carcinoid tumors start from specialized hormone-making cells in the intestine.
Gastrointestinal stromal tumors (GISTs) start from specialized cells in the wall of the colon called the interstitial cells of Cajal. Some are non-cancerous (benign). These tumors can be found anywhere in the digestive tract, but it is unusual to find them in the colon.
Lymphomas are cancers of immune system cells that typically start in lymph nodes, but they can also start in the colon, rectum, or other organs.
Sarcomas can start in blood vessels, muscle layers, or other connective tissues in the wall of the colon and rectum. Sarcomas of the colon or rectum are rare.
