The study of human genetics is not a new concept or practice, having its roots in the early 20th century. Applying the study to medicine came about more recently but can still be traced back to just after World War II. Today, medical genetics has advanced to the point that it is possible to treat genetic diseases, identify if individuals have a predisposition to cancer, and even edit the human genome.
“I think we are part of the revolution,” Dr. Donald Kohn, professor at the UCLA David Geffen School of Medicine and member of the UCLA Broad Stem Cell Research Center, told the Business Journal. “For all these genetic diseases – and there are a couple of thousand single-gene defects in humans – if we can get the genes fixed, we have treatments right at the root cause rather than dealing with symptoms that are five steps away. I would hope that in the future there will be a gene therapy for all of these diseases that can correct the gene in the patients and make them better.”

Molly Lehman, right, a genetic counselor at Long Beach Medical Center’s Todd Cancer Institute, said that genetic testing of patients may determine if they have inherited a predisposition to contracting cancer. By identifying increased risk early on, Lehman said cancer diagnoses would hopefully decrease in the future. (Photograph by the Business Journal’s Pat Flynn)
For the past 30 years, Kohn has been researching and developing a treatment for Severe Combined Immunodeficiency (SCID), which is characterized by ineffective T cells and B cells (types of white blood cells), making the person highly susceptible to infectious diseases. The condition is commonly known as “bubble baby disease” after a young boy suffering from the disorder was outfitted with sterile bubble to live in during the 1970s – the Bubble Boy, David Vetter.
Bubble baby disease occurs when a person is born with bad copies of the gene needed to develop an immune system from both parents, Kohn explained. Without the blueprint to create an immune system, he said that nearly every baby with the disease dies before their first birthday.
New blood cells are produced in the bone marrow. For the last 30 or 40 years, it has been known that SCID could be treated with bone marrow stem cells from a healthy brother or sister who is a match, Kohn said. However, many children do not have siblings, and if they do they may not be a match.
Kohn has been conducting clinical trials for SCID treatments since 1993. Early trials utilized a retrovirus that typically affects mice as a delivery system for the missing gene. A retrovirus is a virus that inserts a DNA copy of its genome into a host cell to replicate. In this process, bone marrow is removed from the patient; then the virus, which has been altered to contain the missing gene, is introduced to the stem cells. The virus inserts the gene into the chromosome, Kohn explained. The stem cells are then intravenously placed back into the bone marrow space where they produce healthy blood cells, ultimately replacing those missing the gene and allowing the patient to develop an immune system.
Clinical trials with this retrovirus were not very effective, resulting in minimal benefits for patients, Kohn said. In 2008, development of the current UCLA Broad Stem Cell Research Center approach utilizing another retrovirus – the human immunodeficiency virus, or HIV – began.
“This class of virus does what we need it to. When they infect a cell, they insert their genes into the chromosome of the cell. Other viruses don’t do that. We learned that HIV was more efficient at getting the gene into human cells,” Kohn said. “Because all the harmful HIV genes have been removed from the virus’s system, there is literally no chance that it can cause AIDS or any problems. It’s just sort of a one-time delivery tool that gets our gene into the cells, and there is no more of the virus left after that point.”
Since 2013, when clinical trials for the current approach began, doctors at UCLA have treated 33 bubble babies using the modified HIV virus. The first 21 patients had a 100% success rate with the procedure being done immediately after the cells were altered. For the next trial, 12 patients had their cells frozen and reintroduced to the body one month later. This process was effective in 11 patients, Kohn said.
Over the course of three decades of work, Kohn noted how greatly the treatment has evolved and improved. He said the current method only mildly affects the babies, since the stem cells being introduced to the body are their own. Because the cells are a perfect match, the body does not try to reject them, and the babies are usually out of the hospital after about a month with a developed immune system.
Recently, UCLA has licensed out the treatment to Orchard Therapeutics, which could attain U.S. Food and Drug Administration approval within a year, Kohn said. The biotech company will eventually bring this and other new therapies to the commercial market, making them widely available, he added.
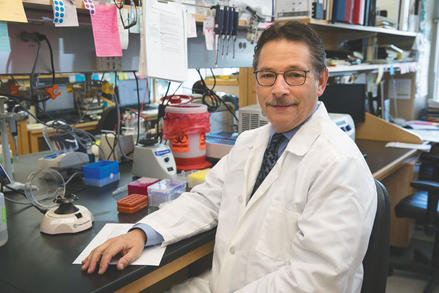
For the past 30 years, Dr. Donald Kohn, professor at the UCLA David Geffen School of Medicine and member of the UCLA Broad Stem Cell Research Center, has been researching and developing a treatment for Severe Combined Immunodeficiency. The treatment uses the HIV virus to correct a genetic code error in babies who have no immune system. (Photograph courtesy of the UCLA David Geffen School of Medicine)
“We’re always careful not to use the ‘cure’ word,” Kohn said. “Even for our bubble babies, until we follow them for 70 years, we can’t guarantee that it’s going to last forever. But so far, we have seen no drop in activity. I think one by one we will find treatments for all genetic diseases.”
Genetic testing of patients can also determine if a person was born with a predisposition for contracting cancer. If a patient has already been diagnosed with cancer, genetic testing can determine if they have an increased risk of another type of cancer. If a person’s genes indicate a predisposition or an increased risk for cancer, doctors are able to make recommendations to minimize the chances that cancer will be contracted. The procedure also enables the detection of cancer in its earliest stages, Molly Lehman, a genetic counselor at Long Beach Medical Center’s Todd Cancer Institute, explained.
Before testing takes place, doctors analyze a patient’s personal and family history to look for certain criteria that may suggest a hereditary predisposition to cancer. If doctors conclude that a patient has increased risk, a saliva or blood sample is taken at the hospital and sent to an outside laboratory where the genetic information is sequenced and analyzed.
“What they are looking for is to see if the patient has a genetic mutation, which is basically like a spelling mistake,” Lehman said. “Our genes are like a computer code that is made up of a lot of different letters, and the laboratory looks through a certain subset of genes . . . and they check for any spelling mistakes, or chunks that are missing.”
The laboratories utilize algorithms and teams of genetic counselors to analyze the genetic data and determine whether or not changes are going to lead to an increased cancer risk, or if they are just normal genetic changes, Lehman said. Each person’s DNA undergoes many changes and mutations that result in the uniqueness of individuals, she explained. Most changes are benign and in no way impact a person’s health. However, certain mistakes or gaps found within particular subsets of genes are associated with increased cancer risk, she noted.
Genetic counselors at hospitals, such as Lehman, assess the results with three possible outcomes: positive for a harmful mutation, negative for a harmful mutation, or uncertain. In the case of a positive result, Lehman said recommendations can be made ranging from lifestyle changes to prophylactic surgery.
For example, if a woman is found to have an increased risk of ovarian cancer, Lehman said it is often recommended that she have her ovaries removed, thereby eliminating the possibility that cancer ever develops. However, these types of permanent recommendations have sparked an ethical debate because it is possible that a particular genetic alteration currently thought to be harmful may not be associated with an increased risk of a disease in the future. If this proves to be the case, there would be a population of people who will have undergone unnecessary surgeries.
Because of these ethical questions, Lehman said the current practice is to treat uncertain results as negative results until such time as they can be confirmed as either positive or negative. When results confirm a harmful mutation, however, she said that there is a high confidence level in making recommendations to patients.
“Looking to the future, we can only assume that, with the more information that we have, the better our classification is going to get and the better our interpretation of these results will be,” Lehman said. “We hope that having this tool at our disposal can potentially reduce cancer diagnoses in these populations that have a very high increased risk for cancer.”
